 The standard treatment of deep vein thrombosis (DVT) is anticoagulants (blood thinners). Following treatment of a clot in the deep veins with anticoagulants, the clot may resolve or, it may turn into scar tissue inside the vein. The scar tissue in the vein can cause either damage to the valves leading to backward flow or a blockage in the vein resulting in poor return of blood to the heart. The blockage in the veins is called chronic venous obstruction.
The standard treatment of deep vein thrombosis (DVT) is anticoagulants (blood thinners). Following treatment of a clot in the deep veins with anticoagulants, the clot may resolve or, it may turn into scar tissue inside the vein. The scar tissue in the vein can cause either damage to the valves leading to backward flow or a blockage in the vein resulting in poor return of blood to the heart. The blockage in the veins is called chronic venous obstruction.
Anticoagulation treatment over time results in clot to either dissolve completely, partially or not at all. Complete recanalization or reopening of the deep vein occurs when the clot resolves entirely without any damage to the vein. More often though, the clot does not completely dissolve but turns into scar tissue within the vein leading to some form of blockage. While DVT and vein damage can occur in any of the deep veins in the leg, the more proximal larger (iliac) veins in the pelvis tend to respond poor to anticoagulation alone.
Recanalization or reopening of the larger clotted iliac veins occurs in about one fourth of patients. The abnormal flow that occurs because of the underlying blockage may result in symptoms of chronic venous disease. Symptoms include heavy legs, swelling of the legs or skin discoloration and damage.
The Diagnosis
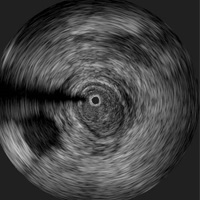 Workup of patients suspected of having chronic venous obstruction includes ultrasound (imaging of the veins using sound wave) in the leg and pelvis. This test is not always good in terms of imaging of veins in the pelvis. Additional evaluation may be required in some patients with either CT (computer tomography) scan or MRI (magnetic resonance imaging). Inconclusive evaluation with the above non-invasive tests or identification of blockage may require use of venography (injecting x-ray dye in the veins) and intravascular ultrasound (a sound wave devise place into the vein to take pictures from the inside) may be needed to determine the extent and degree of blockage.
Workup of patients suspected of having chronic venous obstruction includes ultrasound (imaging of the veins using sound wave) in the leg and pelvis. This test is not always good in terms of imaging of veins in the pelvis. Additional evaluation may be required in some patients with either CT (computer tomography) scan or MRI (magnetic resonance imaging). Inconclusive evaluation with the above non-invasive tests or identification of blockage may require use of venography (injecting x-ray dye in the veins) and intravascular ultrasound (a sound wave devise place into the vein to take pictures from the inside) may be needed to determine the extent and degree of blockage.
Treatment
Open surgical techniques have been used in the past to jump over the blockage in veins and reestablish adequate blood flow back to the heart. This has been replaced with a much less invasive procedure using stents. Venous angioplasty (opening a vein using a balloon inside the vein) along with venous stenting (placing a metal support device inside the vein) helps reopen the blocked vein. Stents do very well in keeping the vein open and in so doing improves the patient’s symptoms. The advantage of the stenting procedure includes minimally invasive, involves little discomfort, good long term results and usually does not have many problems during or after the procedure.
The Procedure
The procedure is performed in a radiology suite using x-ray and contrast dye. A needle is placed into one of the veins in the lower leg after numbing medicines have been given. A wire and catheter (small tube) is then passed up the vein to the place where the blockage is located. Pictures are taken with x-ray dye to visualize the areas of blockage. With some maneuvering of the wire the blockage is traversed. A balloon can then be passed over the wire and blown up to increase the size of the vein. This alone does not keep the vein open and often a stent is then placed from the inside.

